Connect With Us
Blog
Blog
Gout and Gender
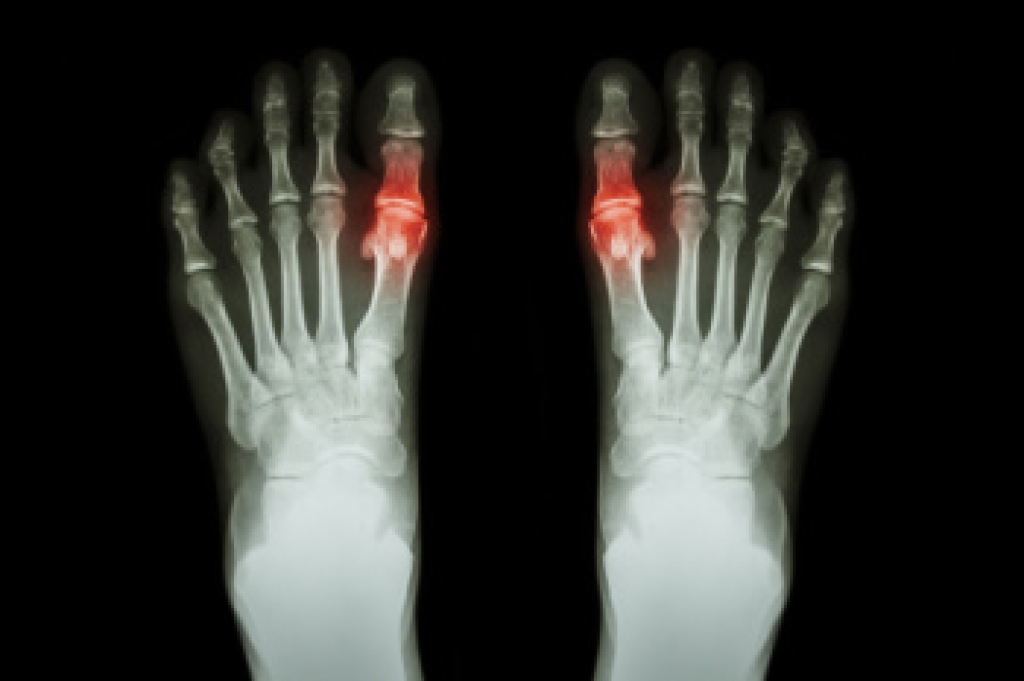
Gout is a form of inflammatory arthritis caused by a buildup of uric acid crystals in the joints, most commonly affecting the big toe. It mostly affects men because they tend to have higher uric acid levels throughout adulthood, while women are partly protected by estrogen until menopause. After menopause, women can also develop gout as uric acid levels rise. Symptoms include sudden intense joint pain, redness, swelling, warmth, and tenderness. Risk factors include obesity, high blood pressure, diabetes, certain medications, and diets high in red meat or alcohol. A podiatrist can diagnose gout, relieve pain, and recommend treatment to prevent future attacks. If you have pain in your big toe, it is suggested that you consult a podiatrist who can provide a proper diagnosis and treatment.
Gout is a foot condition that requires certain treatment and care. If you are seeking treatment, contact one of our podiatrists from Greater Boston Foot Care, PLLC. Our doctors will treat your foot and ankle needs.
What Is Gout?
Gout is a type of arthritis caused by a buildup of uric acid in the bloodstream. It often develops in the foot, especially the big toe area, although it can manifest in other parts of the body as well. Gout can make walking and standing very painful and is especially common in diabetics and the obese.
People typically get gout because of a poor diet. Genetic predisposition is also a factor. The children of parents who have had gout frequently have a chance of developing it themselves.
Gout can easily be identified by redness and inflammation of the big toe and the surrounding areas of the foot. Other symptoms include extreme fatigue, joint pain, and running high fevers. Sometimes corticosteroid drugs can be prescribed to treat gout, but the best way to combat this disease is to get more exercise and eat a better diet.
If you have any questions, please feel free to contact our office located in Plymouth, MA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
The Pain of Morton’s Neuroma

Morton’s neuroma is a painful condition involving irritation and thickening of a nerve in the foot, most often between the third and fourth toes. It is commonly caused by repetitive pressure from tight shoes, high heels, foot structure, or activities that place stress on the forefoot like running or jumping. Symptoms include burning pain, tingling, numbness, or the sensation of standing on a pebble. The foot may look normal from the outside, but it can feel quite painful, especially when walking or wearing narrow shoes. A podiatrist can help by beginning with a detailed history and physical examination, often supported by imaging to confirm the diagnosis. Treatment may progress to footwear changes, custom orthotics, anti-inflammatory care, and injection therapy when appropriate. Early treatment can reduce nerve irritation and prevent worsening symptoms. If you have Morton’s neuroma, it is suggested that you schedule an appointment with a podiatrist for appropriate treatment.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact one of our podiatrists of Greater Boston Foot Care, PLLC. Our doctors will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our office located in Plymouth, MA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot Bone Coordination in Ballet and Podiatric Support

In ballet, the bones of the foot work together to create strength, grace and precise control. Proper alignment allows dancers to move smoothly while maintaining balance and stability. In first position, the feet turn outward from the hips with the heels close together, creating a stable base that requires even weight distribution through the foot bones. In second position, the feet remain turned outward, but are spaced apart increasing the base of support and allowing greater balance, movement and freedom. These positions rely on coordinated function of the bones, joints, and muscles to manage space and control body weight. A podiatrist can help dancers by evaluating foot mechanics, addressing pain, and preventing injury through supportive care. If foot discomfort affects your dancing, it is suggested that you consult a podiatrist who can provide effective relief techniques, enabling you to dance freely again.
If you have any concerns about your feet, contact one of our podiatrists from Greater Boston Foot Care, PLLC. Our doctors can provide the care you need to keep you pain-free and on your feet.
Biomechanics in Podiatry
Podiatric biomechanics is a particular sector of specialty podiatry with licensed practitioners who are trained to diagnose and treat conditions affecting the foot, ankle and lower leg. Biomechanics deals with the forces that act against the body, causing an interference with the biological structures. It focuses on the movement of the ankle, the foot and the forces that interact with them.
A History of Biomechanics
- Biomechanics dates back to the BC era in Egypt where evidence of professional foot care has been recorded.
- In 1974, biomechanics gained a higher profile from the studies of Merton Root, who claimed that by changing or controlling the forces between the ankle and the foot, corrections or conditions could be implemented to gain strength and coordination in the area.
Modern technological improvements are based on past theories and therapeutic processes that provide a better understanding of podiatric concepts for biomechanics. Computers can provide accurate information about the forces and patterns of the feet and lower legs.
Understanding biomechanics of the feet can help improve and eliminate pain, stopping further stress to the foot.
If you have any questions please feel free to contact our office located in Plymouth, MA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Intermittent Claudication and Peripheral Artery Disease

Intermittent claudication is a common symptom of peripheral artery disease, or PAD, and reflects reduced blood flow to the legs during activity. Intermittent claudication is a tight, aching, or squeezing pain in the calf, foot, thigh, or buttock. It typically begins after a certain amount of walking or climbing but eases with rest. As circulation becomes more limited, pain may start sooner, walking distance shortens, and legs can feel weak or cramp. Advanced PAD can cause pain at rest, cold or numb toes, slow healing sores, skin color changes, or shiny skin, which signals higher risk to the feet. Because several conditions can mimic intermittent claudication, a podiatrist plays an important role in evaluation, vascular screening, foot exams, and coordination of appropriate care. For help dealing with symptoms of peripheral artery disease, it is suggested that you make an appointment with a podiatrist for an exam, diagnosis, and treatment.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with one of our podiatrists from Greater Boston Foot Care, PLLC. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our office located in Plymouth, MA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Blog Archives
- 2026
- 2025
- 2024
- 2023

