Connect With Us
Blog

A bump on the bottom of the foot can be caused by several common conditions, including plantar warts, calluses, or a plantar fibroma. Each has distinct causes and symptoms. Plantar warts are caused by the human papillomavirus or HPV, and often appear as rough, grainy growths with tiny black dots. They may be painful when walking. Plantar calluses are thickened areas of skin that develop from repeated pressure or friction, and are typically painless unless they become very thick. A plantar fibroma is a firm, fibrous lump in the arch of the foot caused by a benign tissue growth in the plantar fascia, which may cause discomfort when walking or standing. A podiatrist can examine the bump and determine the exact cause. Treatments vary and may include cryotherapy, trimming thickened skin, orthotics, targeted exercises, or minor surgery, for fibromas. If you have a painful bump on the bottom of your foot, it is suggested that you schedule an appointment with a podiatrist for appropriate treatment.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with one of our podiatrists from Greater Boston Foot Care, PLLC. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our office located in Plymouth, MA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Our feet are arguably the most important parts of our bodies because they are responsible for getting us from place to place. However, we often don’t think about our feet until they begin to hurt. If you have pain in your feet, you need to first determine where on the foot you are experiencing it to get to the root of the problem. The most common areas to feel pain on the foot are the heel and the ankle.
Heel pain is most commonly attributed to a condition called plantar fasciitis. Plantar fasciitis occurs when the plantar fascia, which is the band of tough tissue connecting the heel bone to the toes becomes inflamed. Plantar fasciitis pain is usually worse in the morning, and it tends to go away throughout the day. If you have plantar fasciitis, you should rest your foot and do heel and foot muscles stretches. Wearing shoes with proper arch support and a cushioned sole has also been proven to be beneficial.
Some common symptoms of foot pain are redness, swelling, and stiffness. Foot pain can be dull or sharp depending on its underlying cause. Toe pain can also occur, and it is usually caused by gout, bunions, hammertoes, ingrown toenails, sprains, fractures, and corns.
If you have severe pain in your feet, you should immediately seek assistance from your podiatrist for treatment. Depending on the cause of your pain, your podiatrist may give you a variety of treatment options.

Foot blisters are small pockets of fluid that form when skin is irritated by friction, heat, or moisture. They often appear after long walks, wearing new shoes, or sweaty conditions. Common spots include the heels, toes, and soles. Although they may seem minor, blisters can become painful and even lead to infection if not treated properly. It is best not to pop them unless they are large or painful. Instead, keep the area clean, dry, and covered with a bandage or blister pad. Wearing moisture-wicking socks, well-fitting shoes, and using foot powder can help prevent future blisters. For people with diabetes or circulation issues, even small blisters should be taken seriously. If a blister becomes red, swollen, or does not heal, it is suggested you see a podiatrist for advanced treatment.
Blisters are prone to making everyday activities extremely uncomfortable. If your feet are hurting, contact one of our podiatrists of Greater Boston Foot Care, PLLC. Our doctors can provide the care you need to keep you pain-free and on your feet.
Foot Blisters
Foot blisters develop as a result of constantly wearing tight or ill-fitting footwear. This happens due to the constant rubbing from the shoe, which can often lead to pain.
What Are Foot Blisters?
A foot blister is a small fluid-filled pocket that forms on the upper-most layer of the skin. Blisters are filled with clear fluid and can lead to blood drainage or pus if the area becomes infected.
How Do Blisters Form?
Blisters on the feet are often the result of constant friction of skin and material, usually by shoe rubbing. Walking in sandals, boots, or shoes that don’t fit properly for long periods of time can result in a blister. Having consistent foot moisture and humidity can easily lead to blister formation.
Prevention & Treatment
It is important to properly care for the affected area in order to prevent infection and ease the pain. Do not lance the blister and use a Band-Aid to provide pain relief. Also, be sure to keep your feet dry and wear proper fitting shoes. If you see blood or pus in a blister, seek assistance from a podiatrist.
If you have any questions, please feel free to contact our office located in Plymouth, MA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Blisters are small pockets of fluid that occur on the top layers of the skin for several reasons. Friction, burns, and diseases are all known causes of blisters. Smaller blisters are known as vesicles, while larger blisters are referred to as bulla. The fluid inside the bubble can be blood, pus, or serum; which is a clear liquid that protects the skin. In most cases, blisters are not a major health issue, but they can be an indicator of a more serious condition.
Causes of blisters vary. Blisters are commonly caused by wearing poorly fitted shoes that rub against the foot. However, there are many other causes besides from friction; including burns, sunburn, insect bites, frostbite, poison ivy/oak, chemical exposure, impetigo, eczema, viral infections, and more.
Most blisters heal by themselves and do not require immediate medical care. If you have a blister, do not pop it since this may cause infection; it is advised to put a bandage over the blister to protect it. If the blister is large, causes pain, or if you have a fever, it is recommended that you see a doctor who can provide proper care. Blisters are easy to diagnose, and if considered prudent by the doctor, can easily be drained of fluid with a sterile needle as well.
To prevent blisters on the feet, wear shoes that fit properly and don’t cause rubbing. Socks can help prevent friction and it is recommended that you wear them if you are wearing shoes. Hand blisters can be avoided by wearing gloves during activities that cause friction against the hand. If you have a blister that pops, do not remove the dead skin, wash the area, apply antibiotic ointment, and cover with a bandage. It is okay in most cases to not seek immediate medical care for a blister if it was just caused by friction. However, if the blister causes pain or does not go away, it is suggested that you see a doctor for a diagnosis.

Edema is a condition characterized by the buildup of excess fluid in the body’s tissues, leading to swelling. When it affects the feet and ankles, it often causes them to appear puffy, feel tight, and sometimes become uncomfortable or tender to the touch. This swelling may worsen after long periods of standing or sitting and can make it difficult to wear shoes comfortably. Common causes include poor circulation, heart or kidney conditions, pregnancy, or certain medications. Edema may also result from injuries or inflammation, and the feet and ankles are especially vulnerable due to their position on the body and the effects of gravity. If your feet and ankles have become swollen, it is suggested that you consult a podiatrist who can determine what the cause is, and offer effective relief and treatment solutions.
Swollen feet can be a sign of an underlying condition. If you have any concerns, contact one of our podiatrists of Greater Boston Foot Care, PLLC. Our doctors can provide the care you need to keep you pain-free and on your feet.
Swollen feet are a common ailment among pregnant women and people who stand or sit for extended periods. Aging may increase the possibility of swollen feet and patients who are obese often notice when their feet are swelling too. There may be medical reasons why swollen feet occur:
- Phlebitis - A condition that causes the veins to become inflamed and can also cause leg pain.
- Liver disease - This may lead to low blood levels of albumin which is a protein. This can cause fluid in the blood to pass into the tissues and several areas of the body can become swollen.
- Heart failure - When the heart doesn’t pump properly the blood that is normally pumped back to the heart can pool in the veins of the legs causing swollen feet.
- Kidney disease - One of the main functions of the kidneys is releasing excess fluid in the body. This type of condition can make it difficult for the kidneys to function properly, and as a result the feet may become swollen.
- Deep-vein thrombosis (DVT)- This is a serious condition where blood clots form in the veins of the legs. They can block the return of blood from the legs to the heart which may cause the feet to swell. It is important to be treated by a podiatrist if this condition is present.
Swollen feet can also be caused by bone and tendon conditions, including fractures, arthritis, and tendinitis. Additionally, there may be skin and toenail conditions and an infection may cause the feet to swell. Patients who take medicine to treat high blood pressure may be prone to getting swollen feet.
Many patients elevate their feet to help relieve the swelling and this is generally a temporary remedy. When a podiatrist is consulted the reason behind the swelling can be uncovered and subsequently treated.
If you have any questions please contact our office located in Plymouth, MA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
There are many reasons why patients experience swelling of the feet. It is rather common and may be a side effect of pregnancy or from sitting and standing for most of the day. Gravity could also play a role in the development of swollen feet. It is known that the weight of blood volume in our bodies is exerted on the veins in the legs and feet. The veins may not work as efficiently during the aging process, and this could make the blood flow backward causing swollen feet. Relief may be found when obese patients lose weight, and it may help to engage in compression therapy by wearing compression socks, stockings, or athletic sleeves. This method can release pressure on the feet and ankles which may help to reduce existing swelling. There are patients who have controlled their swollen feet by implementing healthy lifestyle changes. These can consist of reducing salt intake, incorporating a gentle exercise regime into the daily routine, and drinking plenty of fresh water. Swollen feet may be a temporary condition that affects people who travel via airplane or automobile, so it is beneficial to walk as frequently as possible even though it can be difficult. Swelling of the feet can also be indicative of other health issues so it is important to pay attention to any type of chest pain, mental confusion, dizziness, or fever. If you consistently have swollen feet, it is strongly suggested that you consult with a podiatrist who can help determine the cause and how to effectively treat it.

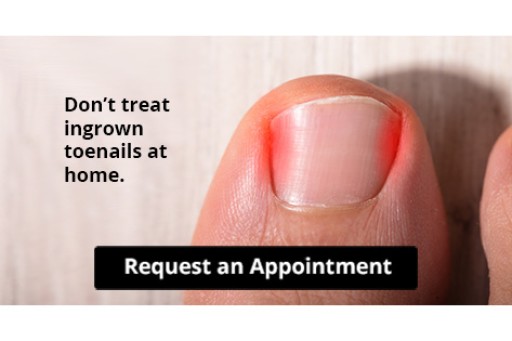
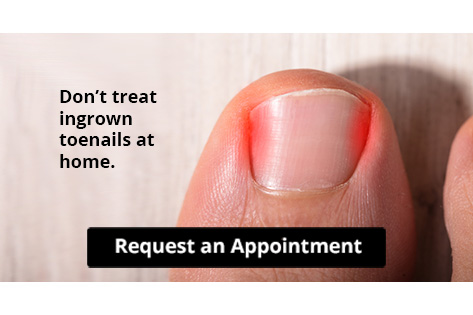
Toenail pain can have many causes, and identifying the source is important for effective relief. One of the most frequent culprits is an ingrown toenail, where the nail digs into the skin and creates irritation or infection. Trauma, such as stubbing your toe or wearing shoes that are too tight, can also lead to pain, discoloration, or even nail loss. Fungal infections may cause the nail to become thick, brittle, or crumbly, often with discomfort or sensitivity. Less commonly, underlying conditions such as arthritis or nerve issues can cause pressure or burning around the toenails. Home remedies may provide temporary relief, but persistent pain should not be ignored. Ignoring the problem can lead to worsening symptoms or permanent nail damage. If you experience ongoing or unexplained toenail pain, it is suggested that you see a podiatrist for a diagnosis and appropriate treatment.
Ingrown toenails may initially present themselves as a minor discomfort, but they may progress into an infection in the skin without proper treatment. For more information about ingrown toenails, contact one of our podiatrists of Greater Boston Foot Care, PLLC. Our doctors can provide the care you need to keep you pain-free and on your feet.
Ingrown Toenails
Ingrown toenails are caused when the corner or side of a toenail grows into the soft flesh surrounding it. They often result in redness, swelling, pain, and in some cases, infection. This condition typically affects the big toe and may recur if it is not treated properly.
Causes
- Improper toenail trimming
- Genetics
- Improper shoe fitting
- Injury from pedicures or nail picking
- Abnormal gait
- Poor hygiene
You are more likely to develop an ingrown toenail if you are obese, have diabetes, arthritis, or have any fungal infection in your nails. Additionally, people who have foot or toe deformities are at a higher risk of developing an ingrown toenail.
Symptoms
Some symptoms of ingrown toenails are redness, swelling, and pain. In rare cases, there may be a yellowish drainage coming from the nail.
Treatment
Ignoring an ingrown toenail can have serious complications. Infections of the nail border can progress to a deeper soft-tissue infection, which can then turn into a bone infection. You should always speak with your podiatrist if you suspect you have an ingrown toenail, especially if you have diabetes or poor circulation.
If you have any questions, please feel free to contact our office located in Plymouth, MA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Ingrown toenails (onychocryptosis) are a common foot ailment and it is very unpleasant to experience. The condition is caused by an increase in pressure from the ingrowth of the nail edge into the skin of the toe. Ingrown toenails commonly cause pain in those who experience them. In some cases, the skin surrounding the ingrown toenail may break which may lead bacteria to enter through and cause an infection. Common symptoms of this ailment include pain, redness, swelling, and warmth around the toe.
An imbalance between the size of the nail and the enlargement of the nail skin edge causes ingrown toenails. This condition is often caused by improperly trimming the toenails. If you are trying you cut your nails, you should always try to trim straight across instead of in a rounded shape. Ingrown toenails can also be an inherited condition and they may also be caused by improper shoe fitting.
Another common cause of the condition is wearing shoes that are either too small or too large. Other causes include poor foot hygiene, obesity, diabetes, arthritis, edema, and fungal infections. There are many risk factors that may make a person more likely to develop an ingrown toenail. Athletes who play “stop and start” sports such as tennis, soccer, and basketball are most likely to have ingrown toenails.
People who have diabetes, a compromised immune system, or poor circulation should immediately seek care from a podiatrist if they have an ingrown toenail. It is also recommended to seek professional assistance if at-home remedies are not successful within a week or if there is persistent pain.
Ankles are joints that connect bones in the feet with bones in the lower leg. They are comprised of bones, ligaments, muscles, tendons, blood vessels, and nerves. The ankle joint allows the foot to move side-to-side, as well as up-and-down.
Ankle pain can be caused by a variety of conditions, but is most commonly due to soft tissue injuries such as ankle sprains and strains.
An ankle sprain occurs when one or more of the strong ligaments that support and stabilize the ankle become overly stretched or even torn if the ankle rolls, turns, or twists awkwardly. Depending on the grade of sprain (mild-moderate-severe), there will be varying degrees of pain, swelling, and restricted range of motion, along with tenderness, bruising, and ankle instability. There may even be an audible popping noise at the moment of injury.
Ankle strains can sometimes produce similar symptoms of pain, swelling, and loss of motion, however, they are due to overly stretched muscles and tendons—not ligaments. Ankle strains may also cause muscle cramps in the feet, calves and shins.
Ankle fractures are another common source of ankle pain and occur one or more of the three bones in the ankle become fractured (broken). These breaks can be stress fractures (due to repetitive stress) or traumatic fractures (due to an acute injury). Depending on where and how severe the fracture is, symptoms can include pain and swelling that can sometimes spread up to the knee, bruising or discoloration, and an inability to bear weight. A visible deformity or exposed bone may occur in severe fractures.
Various forms of arthritis may also cause ankle pain. Rheumatoid arthritis (RA) causes the immune system to attack healthy joints, like the ankle joint, by mistake, causing stiffness and swelling in both ankles. Osteoarthritis occurs when cartilage covering the ends of bones wears down, causing the bones to rub against each other. This results in pain, stiffness, and reduced range of motion in the ankle. Gout is a form of arthritis where excess amounts of uric acid in the bloodstream crystallize and build up on joints, causing severe pain and swelling. Reactive arthritis causes joint pain and swelling in the ankle in response to an infection in another part of the body.
Other forms of ankle pain include bursitis (an inflammation of a cushioning bursa sac between tendons and bone), scleroderma (a thickening of connective tissues), chronic ankle instability (caused by improperly healed ankle sprains), Achilles tendon injuries, flat feet, or an infection in the ankle.