A bunion is a bony bump that forms at the base of the big toe, caused when the tip of the toe lean toward the others. This misalignment is often the result of inherited foot structure, improper footwear, or conditions like arthritis. Risk factors include family history, flat feet, and wearing tight or pointed shoes. Prevention includes wearing shoes with wide a toe box, using supportive shoe inserts, and avoiding high heels. A podiatrist can assess foot structure, recommend custom orthotics, and provide treatment to relieve pain or suggest surgical correction, when necessary. If you are experiencing discomfort near your big toe or notice a visible bump, it is suggested that you schedule an appointment with a podiatrist who can offer relief and treatment tips.
If you are suffering from bunion pain, contact one of our podiatrists of Greater Boston Foot Care, PLLC. Our doctors can provide the care you need to keep you pain-free and on your feet.
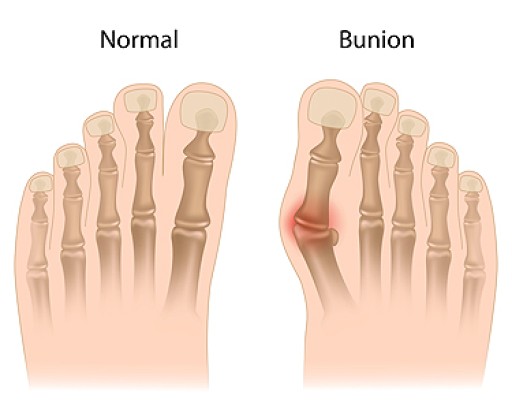
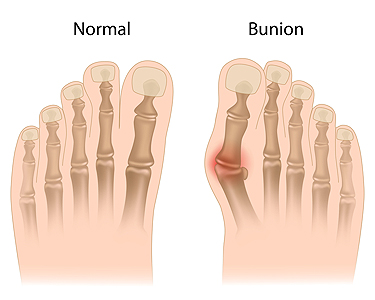
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact our office located in Plymouth, MA . We offer the newest diagnostic and treatment technologies for all your foot care needs.